
is joining VYGON

PEROUSE MEDICAL becomes the Cardio-Vascular and Adult Long term Vascular Access specialist within VYGON’s group

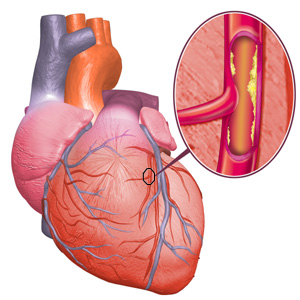
The heart (=myocardium) is a hollow pear-shaped muscular organ located between the lungs, in the middle of the chest, immediately behind the sternum. The volume of the adult heart is similar to that of a fist. It consists of 4 cavities: 2 atria (right and left) and 2 ventricles (right and left). The atria and ventricles retract and relax alternately to allow them to fill with blood and eject blood throughout the body. The heart is physiologically infatiguable provided it receives sufficient amounts of oxygen and nutrients. It is normally fed by 2 arteries called coronary arteries, the name of which comes from their arrangement in a crown around the heart. These are the left coronary artery and the right coronary artery, which supply the corresponding ventricles.
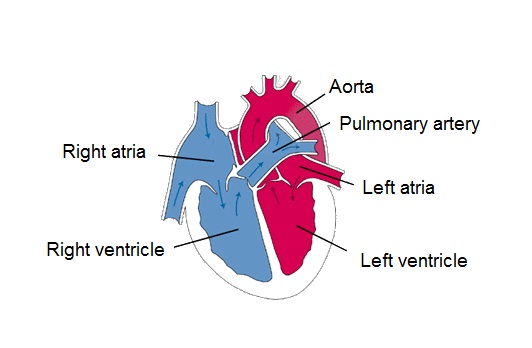
Ventricles and atria of myocardium
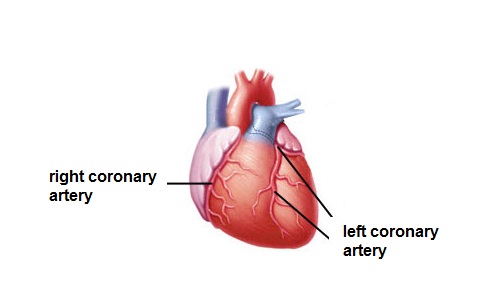
Myocardial coronary arteries
Coronary artery disease affects almost 3 million people in France. It is due to the narrowing of the diameter of one or more coronary artery(ies) usually due to local thickening of the arterial wall, and called stenosis.
Thickening of the arterial wall due to an accumulation of fats (cholesterol) is initially localised, forming an atheromatous plaque. The plaque then changes through fibrosis and calcification to form atherosclerosis. The plaques have an increasing tendency to develop with increasing age. Over time the lumen of the artery narrows, myocardial blood supply and therefore oxygen becomes inadequate for its needs and the oxygen deficiency makes it impossible for the myocardium to function normally. At an advanced stage, the obstruction can be total and permanent. This is very often due to rupture of an atheromatous plaque leading to the formation of a blood clot which blocks the artery. The blood circulation is then interrupted in a particular area leading to death of cardiac cells in this area. This is myocardial infarction.
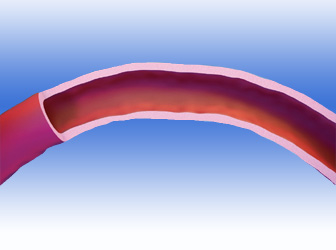
Normal artery
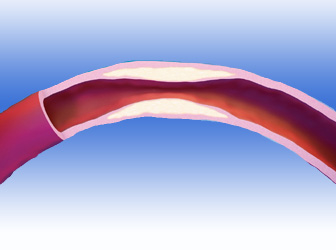
Stenosed artery
Angina is usually the 1st symptom of coronary artery disease. It may involve excruciating constrictive pain (angina) usually located in the middle of the chest and occasionally radiating to the jaws and arms. The site of the pain may however vary and it may be associated with respiratory difficulties. The sensation of pain or discomfort in the chest develops with exercise or more generally when the heart rate increases and is rapidly relieved (in less than 3 minutes) by stopping the exercise which caused it and/or by taking glyceryl trinitrate.
‘Stable angina’ is characterised by reproducible symptoms at a given level of effort and the level of effort and is related to the degree of narrowing of the diameter of the coronary artery which restricts the blood flow. In ‘unstable angina’ the symptoms are not reproducible at the same level of effort, the pain is liable to occur with increasingly lower levels of exercise or persist after the exercise has been stopped, or even at rest.
Unstable angina is an indication of an imminent risk of arterial obstruction and requires a specialist opinion. Centre 15 (the urgent emergency service) must be called immediately without delay if the pain is prolonged (15 minutes) and excruciating with a feeling of imminent death and is accompanied by sweating, nausea or vomiting which are the premonitory signs of myocardial infarction. Myocardial infarction can be avoided through the emergency care teams, the cardiology intensive care unit and the interventional cardiology group provided that the intervention takes place within 6 hours after the onset of symptoms begin.
The absence of angina does not guarantee the absence of myocardial ischaemia in the following situations:
The ischaemia may be revealed by its cellular effects which usually precede the angina.
The main risk factors for coronary artery disease are:
The secondary risk factors for coronary artery disease are:
Treatment involves 2 components. The 1st component is preventable and involves correcting or compensation for risk factors (improved lifestyle etc). The 2nd component is curative and is designed to reduce or remove the ischaemia or its consequences:
The investigation involves taking radiographic films of the coronary arteries which supply the heart.
A contrast medium which is opaque to X-rays is injected directly into the coronary arteries through a catheter which is introduced through the groin or wrist. Continuous radiography is taken during the injection and filmed to visualise the appearance of the arteries.
Morphological examination is used to confirm whether or not stenosis is present, liable to cause chest pain or even myocardial infarction if the arteries are completely blocked. This examination is supplemented by measurement of pressures in the vessels and cavities of the heart in order to assess whether they are functioning normally or pathologically.
The procedure is almost painless and is generally performed under local anaesthesia by a cardiologist who is specially trained in this investigation. It usually lasts between 15 and 20 minutes and its results are immediate.
As a result of the coronary artery investigation the cardiologist can decide the best treatment, either immediately or after joint discussion with other specialists including the cardiac surgeon. The treatment offered may be:
Approximately 260,000 coronary angiograms are performed in France each year and approximately 6 million across the world.
This investigation is used to assess the extent of narrowing of one or more coronary arteries or for a threatened myocardial infarction which may present as:
The investigation may be contra-indicated (unless the patient benefit takes priority over the contra-indication) or is deferred in the following situations:
For a planned investigation, you will return to the hospital the day before or on the morning of the investigation which will be performed after a blood screen and electrocardiogram. Some medical treatments may be stopped and others may be started in order to perform the procedure. Do not forget to report any allergies (including iodine). You will be told how the investigation is performed and will be asked to read and then sign the ‘informed consent form’ to give your agreement to the investigation that is being offered to you.
You will need to have been fasting for 4 h for solid foods and 2 h for liquids before the investigation.
You will be shaved widely around the puncture site for the artery used, in your wrist or groin.
You will be taken into the investigation room (catheterisation room or interventional cardiology suite).
In this room you will lie down on the examination table with nothing on your back and your arms lying alongside your body. You will be covered with a sterile drape. Beneath the table a tube emitting x-rays coupled to a receiver which is placed in front of your chest, will allow your investigation to be performed. The receiver moves around your chest to record the images filmed. You should not move during the injections.

Catheterism laboratory
Your heart rate and blood pressure will be recorded throughout the investigation. An intravenous catheter will be inserted into your forearm: this is used to inject medicines if necessary during the procedure.
After carefully disinfecting the puncture site, the cardiologist will administer a local anaesthetic. The radial artery is punctured at the wrist and the femoral artery in the groin. The choice of puncture site depends on the features of the artery, patient body morphology, type of investigation being performed, catheters being used and the doctor’s usual practice and/or experience. It may not be possible to perform the investigation from the initial approach used (abnormality of the arterial path, small calibre etc) and the approach may need to be changed during the investigation.
After the local anaesthesia the doctor will puncture the artery using a small needle in order to position a small watertight tube to allow the catheter to pass through. A catheter will be introduced into the artery, advanced to the heart and positioned just at the origin of a coronary artery. The artery is then visualised by injecting contrast medium. The cardiologist will check whether or not there is a stenosis in the calibre of the artery. The investigation is repeated in different views to avoid missing a stenosis hidden by the thickness of the vessel. The same procedures are performed to study the secondary coronary artery and, possibly, some other arteries or bypasses if these are present. The filmed appearances are digitalised and recorded in order to be studied in more detail.
The investigation may be combined with left ventriculography, which is a radiograph taken of the left ventricle after injecting high flow contrast medium. The injection usually causes a mild sensation of warmth which spreads for a few seconds from the chest to the lower parts of the body (and sometimes gives a feeling of passing urine). The aim of this investigation is to assess the morphology and contractile quality of the left side of the heart. Once the investigation is finished the catheters are removed.
If the puncture has been made through the radial artery a dressing or compressive band will be applied to your wrist at the level of the puncture site to avoid any bleeding. This compression is kept in place for 2 – 5 hours and is gradually loosened until the dressing is removed. You will have to avoid moving your wrist during this time.
If the puncture is made through the femoral artery the doctor will apply manual pressure to the puncture site for around 10 minutes until the bleeding stops and a local dressing will be applied using an adhesive elastic bandage. An arterial closure system may be used avoiding manual compression and bandaging although this needs the thigh to be kept strictly immobile to avoid forces on the artery and the risk of secondary bleeding.
The doctor who performs the investigation will give you an initial description of the results. Your cardiologist will be kept informed of the results for your continuing care and treatment. The hospitalisation generally lasts between 24 and 48 h.
Coronary dilatation (angioplasty with or without stenting) may be performed immediately after the coronary angiography although it may be done later (either to consider the strategy to be used or to give essential treatment before the procedure). If the angioplasty is performed only a short time later the small watertight tube for the catheter to pass through may be left in place at the puncture site.
Complications are relatively rare and usually not serious:
More serious events can however happen usually because of the disease itself:
The risks of coronary angiography are usually far less than the risks of progression of the coronary artery disease itself.
The irradiation doses from the X-rays used for this investigation are normally negligible:
the doses delivered are limited to what is strictly necessary, monitored (measured during the investigation) and recorded in your records. The true danger from irradiation is the cumulative dose received: and therefore the dose delivered by all the investigations that you have during your life (beware of the dose delivered by CT scans), how often these are repeated and the areas irradiated.
You should remember that you should not bend your wrist or lift your thigh, depending on the arterial approach used for the investigation, to avoid any risk of bleeding. Drink plenty (1.5 to 5 litres) to help to remove the contrast medium that is injected during the investigation. If you feel warmth in the dressing or where the catheters were introduced, or pain in your leg or foot, or arm or hand, tell the doctor or nurse.
If you develop chest pain, fever or malaise during the days after the investigation consult your doctor.
Angioplasty is one of the reference treatments for coronary artery stenoses. The walls are separated by inflating a balloon and the artery is returned to its initial diameter. The result is usually consolidated by inserting an appropriate stent.
Like coronary angiography, angioplasty is performed in an interventional catheterisation suite. It may be performed at the time of coronary angiography or in the days afterwards.
In an emergency situation (myocardial infarction), the patient may be taken by the emergency services straight to the hospital for an angioplasty to be performed as soon as possible.
The procedure is performed by an interventional cardiologist.
The procedure is indicated when a stenosis has been found in one or more coronary arteries during the coronary angiography and is thought to be causing poor perfusion of the heart.
In the same way as the preliminary coronary angiography, the potential risks and benefits of the process will be explained to you and you will be asked to confirm your agreement by signing the ‘informed consent’ form.
You will need to have been fasting for 4 hours (neither eating or drinking) before the procedure.
Some medical treatments may be stopped in order to perform the procedure.
Other treatments may need to be started (platelet anti-aggregants) in some cases. You will have already been shaven at the arterial puncture site.
The procedure process is exactly the same as for coronary angiography until the catheter is positioned at the origin of the coronary artery which is to be dilated (see above). The cardiologist will inject the contrast medium into the coronary artery which is to be treated in order to correct the stenosis or stenosis found.
A very thin guide wire will be introduced into the coronary artery which the cardiologist will use to break through the stenosis. The balloon intended to dilate the stenosis is located at the end of a very thin tube which slides along this guide to the stenosis. The inflated balloon crushes the coronary artery wall returning it to its initial diameter. Whilst the balloon is being inflated you may experience discomfort in your chest, or even a pain exactly the same as the angina attacks, as inflating the balloon obstructs the blood flow. In this case the pain will disappear as soon as the balloon is deflated. Sometimes a single balloon dilatation is enough to unblock the artery. Usually the dilatation is combined by positioning a stent which fits the size and shape of the artery and which maintains the artery’s diameter. Only the stent remains in place at the end of the procedure: the balloon, guide wire and catheter are removed.
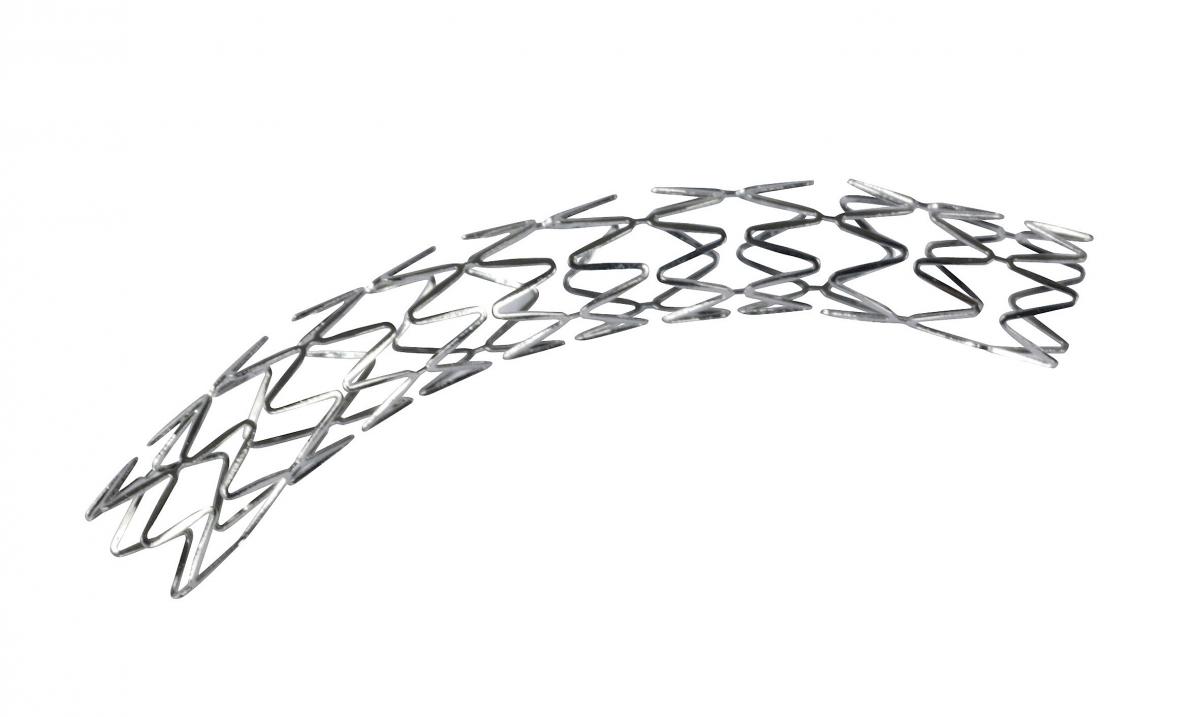
Stent (endoprosthesis)
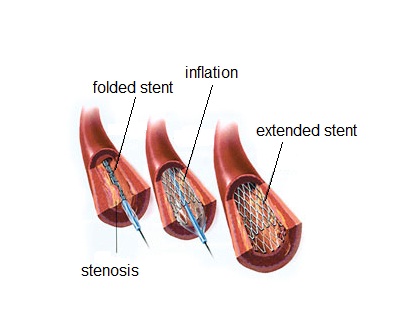
Positioning a stent in the coronary artery
Very rarely (less than 1% of cases), the angioplasty procedure does not achieve a satisfactory result and may be repeated later or the treatment strategy may be reviewed (medical treatment or bypass surgery).
Usually it is immediately successful. Angioplasty is always combined with continuing medical treatment designed to reduce progression of the coronary artery disease.
Restenosis may occur (in approximately 10% of cases) within 6 months after the angioplasty procedure. If the risk of restenosis appears to be high, a stent covered with a medicine may be chosen to reduce this risk rather than plan a stent not containing an active substance (‘uncoated stent’). This option (which is regulated in France by strict criteria for cost reasons) requires longer term treatment to prevent the risk of clot formation and is a contra-indication for any surgery (except of course for urgent life saving surgery) for 6 months after it is implanted.
At the end of the procedure and after the materials have been removed the arteries are compressed or closed by a local device (resorbable collagen closure or automatic suture) in the same was as after coronary angiography.
After the procedure you will remain in the recovery room and then taken to your bedroom or intensive care where your electrocardiogram will be monitored.
You will be able to eat and drink after the end of the procedure.
The interventional cardiologist will give you an initial description of the results and instructions to follow later. Your cardiologist will be kept informed of the methods used and the results of the procedure and will be able to continue your follow-up and treatment.
The hospitalisation usually lasts between 24 and 48 h.
The complications (rare and often not serious) are the same as those of coronary angiography but also include a risk of rupturing the artery which is being treated. You should consult your doctor or call the centre which performed the procedure if you develop chest pain, fever or malaise in the days after the procedure.
You should remember that you must not bend your wrist or leg, depending on where your bandage is, in order to avoid any risk of bleeding. Drink plenty (1.5 to 5 litres) to remove the contrast medium that was injected during the procedure.
Report any chest pain or pain at the puncture site (or in your hand or leg) or a feeling of warmth in the dressing.
Follow the instructions given to you at the end of the procedure. You can start taking regular physical activity very soon unless you are advised not to, in which case you will be told why. It is essential to continue treatment and control ‘risk factors’. Your cardiologist will follow you up at intervals.